Authors: Marisa Vella, Francesca Micallef, Alan Sciberras Narmaniya
Published Online: 21-12-2022 | Sourced From: MCAST Journal of Applied Research & Practice Volume: 6, No.: 4, 2022
Abstract: Despite consensus about the preventable nature of dehydration, it remains particularly prevalent among older adults residing in residential care home settings. The aim of this study is to explore current hydration practices in residential care homes in Malta. An exploratory qualitative approach was adopted to provide an in-depth understanding of staff’s practices for supporting residents’ hydration in care homes for older adults. Following a feasibility study to increase the overall methodological rigour, thirty-one staff participants across six residential care homes, covering all the six regions of Malta, participated in either face-to-face or online semi-structured interviews. Data was analysed through open coding, followed by axial coding. Peer debriefing amongst the research team was carried out until agreement was reached about the final themes. Three main themes emerged from the data: culture of promoting fluid intake; challenges in supporting older adults to achieve optimum hydration; and hydration practices and approaches. A hydration-promotion culture was evident across all care homes. However, there was a lack of consistency in monitoring hydration and daily fluid targets which emphasises the need for staff training and implementation of clear and accessible guidelines, policies and/or procedures in relation to hydration care within residential settings for older adults. Future research attention should focus on establishing an evidence-based approach to monitoring hydration status and identifying residents at risk of dehydration. Difficulty in monitoring the fluid intake of independent residents was highlighted and we contend that this group of residents should not be overlooked in view of the risk of dehydration. Employing robust and rigorous methods to establish the effectiveness and implementation of innovative approaches would help in making valid contributions to the local evidence base on hydration care in residential care settings.
Keywords: fluid intake; hydration care; older adults; residential care
Introduction
Dehydration is a serious health problem for older adults and is associated with increased morbidity, mortality, and hospitalisation (Bunn and Hooper 2019; Lesnik and Bevac 2015; Murray 2017). Projections indicate that Malta is one of the fastest ageing countries in the European Union (Formosa 2019). This, together with the impact of the COVID-19 pandemic, places further economic burden on healthcare resources (OECD 2021). There is widespread consensus that dehydration, particularly due to insufficient fluid intake (Lesnik and Bevac 2015), is preventable and reversible (Bunn, Hooper, and Welch 2018; Robinson and Rosher 2002; Simmons, Alessi, and Schnelle 2001; Wotton, Crannitch, and Munt 2008;). Even so, it remains a common problem in residential care settings (Hart, Marsden, and Paxman 2020) and is associated with poor outcomes and low quality of life for older people (Hooper et al. 2016; Lesnik and Bevac 2015; Paulis et al. 2018; Vandervoort et al. 2013; Wolff, Stuckler, and McKee 2015; Wotton, Crannitch, and Munt 2008).
Older people are vulnerable to dehydration due to physiological changes in the ageing process, and this can be exacerbated by many disease states and mental and physical frailty (Wolff, Stuckler, and McKee 2015). Thirst in older people may not be relied on as an indicator of dehydration (Shaw and Cook 2017) and residents are often concerned about the risk of incontinence resulting in restricting their fluid intake (Wilson et al. 2019). For older people living in residential care, this means that they need to rely on care home staff for support to meet their daily fluid requirements. Although European guidelines recommend a daily fluid intake of 2.5 litres through food and drink for men and 2 litres for women (European Food Safety Authority 2010), literature indicates that residents in care home settings have inadequate fluid intake (Gasper 2011; Woodward 2007). Research on hydration in nursing homes in Malta is limited. In 2016, for most patients having challenges with being discharged from the island’s main acute hospital, it was noted that the most common reasons for their admissions were confusion or lethargy and dehydration (Formosa and Farrugia Jones 2017). Although dehydration was a primary reason for 3.5% of admissions between 2018 and 2020 (Hospital Activity Analysis 2021), this figure excludes admissions that report dehydration as a secondary cause and does not consider older adults who are treated for dehydration in residential care settings.
Research on strategies aimed at promoting hydration in residential care settings remain heterogenous (Vella, Sciberras Narmaniya, and Micallef 2021). Environmental stimuli, drinking-related activities, promoting choice and preference, use of specialised equipment and increased frequency of routine offers of drinks, have all been cited as successful strategies in improving hydration intake to meet the daily requirements of residents (Allen, Methven, and Gosney 2013; Cook et al. 2019; Hart, Marsden, and Paxman 2020; Kingston 2017; Oates and Price 2017; Robinson and Rosher 2002; Wilson et al. 2019). However, it is widely recognised that assisting residents to drink is a time-consuming task and staff often have to choose between other essential care activities (Gasper 2011; Godfrey et al. 2012; Mentes 2006). In residential care, this can be exacerbated by inadequate staff training and lack of awareness of the importance of hydration (Cook et al. 2019). Preliminary findings from the related feasibility study also indicated that staff often find it difficult to monitor the fluid intake of independent residents (Micallef, Vella, and Sciberras Narmaniya 2021), placing this particular group at greater risk of dehydration.
Given the current state of knowledge on hydration practices in Malta’s older population, and the pressures placed on current healthcare services, it is deemed important to contribute to this area of research. Such insight could be valuable in addressing current challenges and make recommendations for reducing the incidence of a disease which is preventable. Following the feasibility study, the overall aim of this main study was to explore current practices of staff regarding the hydration intake of older people living in homes in Malta, utilising a larger sample from different care homes. The detailed objectives of this research were: (1) to explore practices by staff working in care homes for older people in Malta in relation to the assessment of residents’ hydration requirements and support required; (2) to explore practices to maintain and promote sufficient fluid intake; and (3) to investigate practices to monitor daily fluid intake and dehydration of care home residents. An exploratory qualitative approach was particularly valuable in providing in-depth qualitative data of existing hydration practices in residential care homes for older adults. This approach was best suited to address the study objectives and gain a deeper understanding of the complexity of how staff assess hydration requirements, the practices to maintain and promote sufficient fluid intake; and how they monitor daily fluid intake and dehydration of residents.
Materials and Methods
Study Design and Study Population
An exploratory qualitative approach was adopted to provide in-depth qualitative data of existing hydration practices in residential care homes for older adults. A feasibility study was initially carried out (Micallef, Vella, and Sciberras Narmaniya 2021) to obtain preliminary data and a thematic coding framework for data analysis. This process allowed for the evaluation of the selected data analysis method and an increase in the overall methodological rigour of the study. Following this, convenience sampling was used to recruit six public-private-partnership care homes for older people, covering all the six regions of Malta (Table 1). Residential homes providing longterm care for older people aged 65 and over, and whose proprietor and manager agreed to staff being invited to take part in a research interview, were included. Thirty-one staff participants across the six care homes were then recruited in a purposive way to obtain a heterogenous sample including different job designations, gender, and nationalities (Table 2). Staff were included in the study if: (1) the individual worked in one of the consenting registered care homes, (2) was responsible for providing residents with drinks and/or supporting residents to drink fluids, and (3) was willing to take part in a research interview.
Data Collection and Data Analysis
A combination of face-to-face and online semi-structured interviews were carried out individually with staff until data saturation was reached in each home. The interview guide was adapted from a previous study undertaken by Cook et al. (2019) which explores hydration practices in residential care homes in the UK. Permission to make use of the interview guide was sought and obtained from Dr Glenda Cook (Northumbria University) and her team. All interviews were recorded and conducted in either English or Maltese, with the latter being translated following transcription. All interview transcripts were submitted to open coding, where the research team went over the data line by line and allocated codes according to the coding framework generated from the feasibility study, whilst looking for any new codes that might have emerged from the new dataset. As part of the process of axial coding, all coded data was merged to identify relationships of codes between the sites and interviews (Braun and Clarke 2006). Each transcript was verified independently by each member of the research team and peer debriefing was undertaken at each stage of analysis to improve the study’s reliability and credibility. Discussions and revisions to the thematic coding were undertaken during peer debriefing meetings until all members of the research team agreed on the themes. This process allowed for an overall view of hydration practices in the study care homes, whilst still understanding any important differences in individual study sites (Micallef, Vella, and Sciberras Narmaniya 2021).
Ethical Approval
Ethical approval was granted by MCAST’s Research Ethics Committee (Reference number: IAS05_2019) and study procedures complied with institutional ethical guidelines. Written approval was sought from and granted by the manager/director of each residential home. Written informed consent was gained from participating staff prior to conducting the interviews. Anonymity was maintained using codes in the presentation of findings. The coding system was only known to the research team and kept secure and separate from the rest of the data.
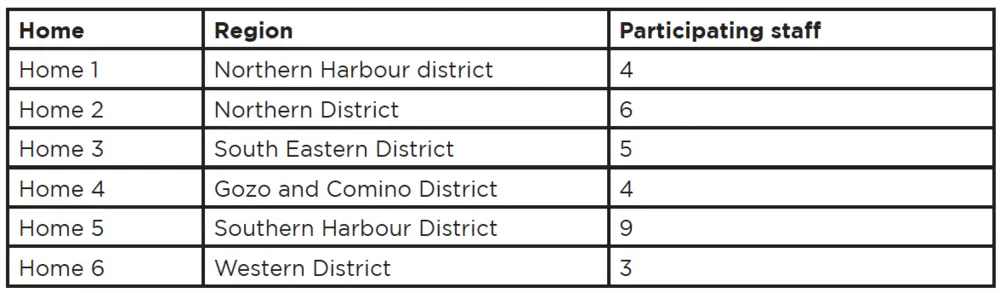
Table 1: Participating Care homes
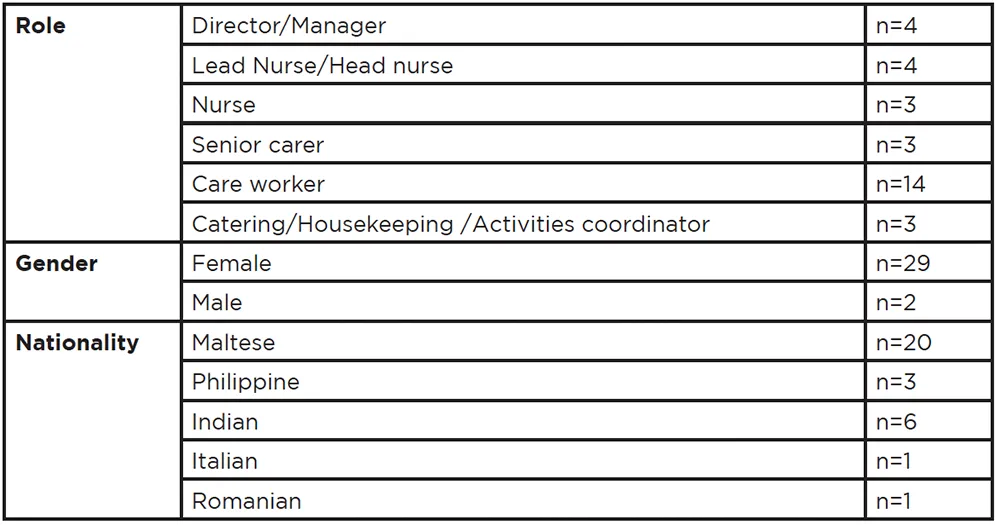
Table 2: Participant Characteristics
Results
Three central themes and 13 sub-themes emerged from examination of the data (Figure 1).
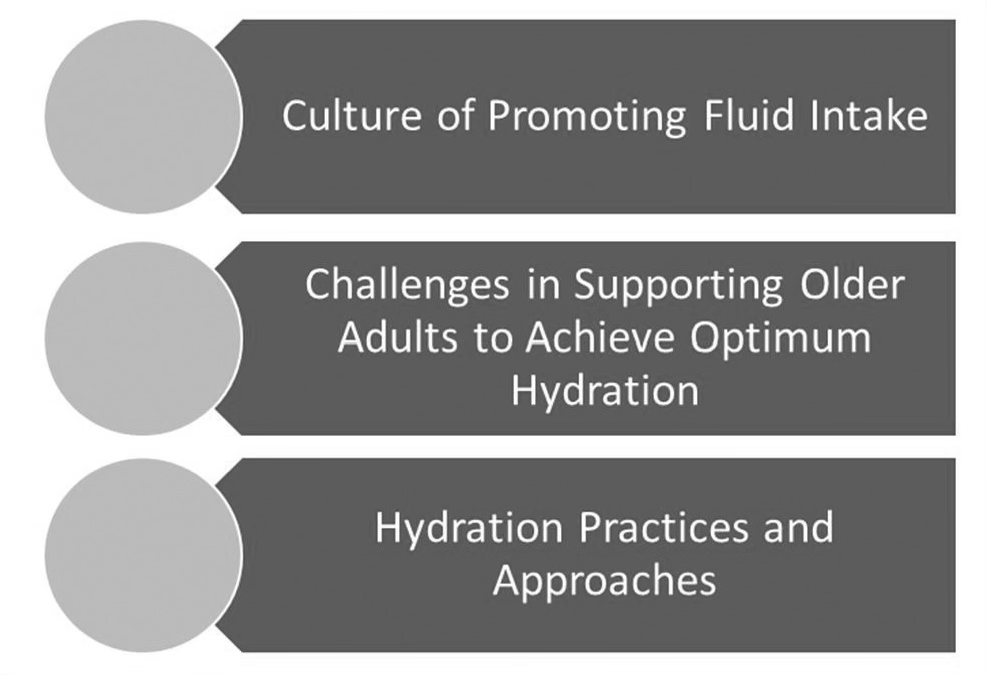
Figure 1: Central themes
Theme One – Culture of Promoting Fluid Intake
The importance of promoting fluid intake was firmly highlighted through the routine provision of fluids. Participants explained that although they do not have policies or guidelines that focus on hydration practices, there is an awareness amongst care home staff on promoting fluid intake and they follow a structure and fixed times to provide drinks. Participants also emphasised the importance of avoiding adverse events, such as episodes of dehydration.
No guidelines …. this is an individual clinical decision. (Participant 15 – Nurse)
Many participants, particularly carers, highlighted that promoting hydration was part of their pre-qualification training and noted that although other training opportunities are provided in some of the care homes, no training or courses had been provided with regard to hydration care practices. Recognition of signs and symptoms of dehydration were notably based on familiarity with the residents. In addition, the daily fluid intake target for a resident with no restrictions varied from 500 – 3,000 millilitres.
Yes, you need to drink 7 to 8 cups, in winter 5 to 7. Each cup has 100 mls. (Participant 9 – Nutritionist)
3 litres if I’m not mistaken or 2…3 litres or 2? (Participant 21 – Care worker)
Processes relating to adverse events focused on avoiding dehydration and the management of residents who become dehydrated. Essentially, when a resident persistently refuses oral intake of fluids, they are referred to the acute care setting, often the hospital.
If a resident will not eat or drink, will refuse one day, let’s say we try for this day, then the second day already in the afternoon we call the ambulance and send them to Mater Dei…because then they will be dehydrated. (Participant 1 – Home Manager)
Episodes of dehydration were noted amongst most homes to be an event which staff take very seriously. Care home staff demonstrated a firm belief that if the residents are kept hydrated and there are minimal episodes of dehydration, that this is a benchmark and indicator of the quality of care they provide.
The most important thing that I always stress is that it would be a shame on us, personally, to get to the point that a resident ends up in a dehydrated state…..We work at not getting there. We do our utmost to prevent it rather than treat it. To be honest, when a nurse tells me that a resident got dehydrated, I say shame on us. (Participant 12 – Lead Nurse)
It’s not nice that, you know that you’re sending someone to hospital because of dehydration…. Because if you send them for dehydration, that means that you’re not taking care of them. (Participant 23 – Care worker)
Theme Two – Challenges in Supporting Older People to Achieve Optimum Hydration
Dependency, cognitive impairments resulting from dementia, refusal to drink, and language barriers where the salient challenges reported with regard to supporting older adults in achieving their hydration requirements. Refusal to drink was attributed to several reasons, ranging from behaviour, the type of drink offered, and issues related to continence.
… those who have the thickener, and they can’t stand it that they have the thickener…. and they wouldn’t want to drink only water on its own…. (Participant 22 – Care worker)
Residents who are dependent were noted to require more attention in achieving their hydration requirements and ensuring they are drinking enough. It was also noted that independent residents are seen to be able to manage on their own and therefore are less of a concern with regard to achieving their hydration requirements. However, participants acknowledged that it is more difficult to monitor the fluid intake of independent residents.
…. our focus is not on them (independent residents). Yes, yes, we are trying to focus on them, but more with the demented residents… the independent residents can walk right? They can go to fill their glass or their empty bottles with water or a drink. (Participant 3 – Care worker)
We distribute water in the lobby or in the rooms, you know. Those who are independent, it’s more… Sometimes it’s difficult for those who are independent because you don’t know how much they are drinking. (Participant 20 – Care worker)
Non-native Maltese speakers noted challenges linked to language barriers since the vast majority of residents are native Maltese speakers. This was particularly prominent when focusing on specific care needs, such as providing hydration, prompting residents to drink, and dealing with challenging behaviour. Residents living with dementia have specific needs. Participants highlighted that they require assistance to drink, attention for swallowing difficulties, including consistency of food and drinks, prompting and observation. Participants also noted that, as a result, providing care to these residents is time-consuming and challenging. A sense of wanting to do more was also noted amongst participants.
Those residents who have dementia are given a lot more attention…… We would like to do more, especially for those residents who have dementia. (Participant 8 – Nurse)
Theme Three – Hydration Practices and Approaches
Hydration practices and approaches were categorised into personalised care planning, offering drinks, and supporting and encouraging drinking. Personalised care planning was reported as an important aspect of hydration care that addressed individual preferences, consideration of medical conditions, assessment and setting daily hydration requirements for residents, as well as reviewing the fluid intake of residents. A number of indicators were identified by participants to determine appropriate fluid intake. These ranged from cognitive abilities, monitoring, blood analysis, and seeking feedback from residents. It was also noted that participants monitor water consumption through documentation, as well as stocks of water bottles.
Yes, because there are residents who never liked tea, for example, who will only drink coffee. So yes, we offer coffee. (Participant 1 – Home Manager)
We ask residents if they are drinking or not and to give us a rough estimate of the actual content drunk. We try to give them bottled water and so we try to measure in terms of the amount of a small bottle. (Participant 15 – Nurse)
Offering drinks during set times and prompting residents to drink beyond the routine or care home timetable were prominent strategies participants spoke about to maintain adequate fluid intake for their residents. All care home staff provided a breakdown of the routine observed within their respective home with regard to the provision of drinks and the allocated times throughout the day. Some homes noted that they have carers focused on providing drinks and assisting residents to drink throughout the day. Lifestyle considerations, as well as an awareness for the types of drinks offered, were also considered. There was a strong focus on water intake and many participants put a high emphasis on the availability, provision, and consumption of water.
We as carers give coffee and tea three times per day. In the morning at 7am, in the afternoon at 2pm, and at night at 7pm. We also encourage the residents to have soup. We provide orange juice or water twice for lunch and dinner. We also make rounds with water in case someone does not have water on the bedside table. (Participant 11 – Lead Carer)
We need to take all opportunities to promote hydration, even when we distribute the medications, we give them a full glass of water and not just enough to swallow the tablets well. (Participant 8 – Nurse)
At 11am they come in for lunch, so we give them water again, we serve them water, they come in for the first sitting, then the second sitting…we all serve them water … (Participant 20 – Care worker)
Regular prompting was seen as an important aspect in supporting and encouraging residents to drink. Strategies reported by participants included offering a range of drinks that residents prefer and offering food with a high fluid content.
…..if a resident does not like water we give them something else like orange juice or milk. (Participant 11 – Lead carer)
Hydrating is not only via water. It is in the food you eat. Among the food they’re eating there are a lot of vegetables. It’s all fresh vegetables. This is hydrating too. (Participant 9 – Nutritionist)
Familiarity with the elderly was noted to be another key aspect in promoting hydration. Social interaction, humour, and therapeutic interactions all had a positive impact on supporting residents to drink. On the other hand, the visiting restrictions due to the COVID-19 pandemic negatively affected the mood of many residents.
When they eat in the dining room they eat more. They see their peers and eat more. We encourage them with the activities and outings too when these are possible, by saying its important to eat everything cause now we have the outing for example. (Participant 9 – Nutritionist)
The relatives weren’t visiting and some of them who weren’t seeing the relatives didn’t want to drink, they didn’t want to eat, and with most of them it was like they were going into depression, so that was the problem. (Participant 7 – Home Manager)
The involvement and contribution that relatives make in promoting fluid intake was also highlighted. Staff encouraged families to bring drinks and offer drinks when visiting. This was often a successful way of increasing the fluid intake of residents.
The relatives bring them juices and other drinks and the residents tell us that I will drink this because my daughter brought it for me. (Participant 9 – Nutritionist)
The impact of drinking activities in promoting hydration was also reported in the majority of homes. Most homes provide celebratory drinks in relation to the respective village feasts and for Christmas and Easter. In addition, most homes also have regular high teas and tomblas, where tea or coffee are free-flowing.
In summer for example because of this, on Thursday we organise a party with ice-cream and the ice-cream van like the old days, and we put on music. I buy them the containers in the form of cup like the ones the ice-cream van has, and we give them a scoop of ice-cream each followed by a glass of water. They all drink. (Participant 9 – Nutritionist)
We have afternoon high teas where each level, we do it on a different week because you can’t do them all together. (Participant 29 – Lead nurse)
Participant responses also highlighted measures in place to promote a drinking-conducive environment. These varied from vending machines, promoting proper hydration with medications, accessibility to kitchenettes, access to common area fridges, frequent distribution of water, availability of drinks in the residents’ own space, and availability of filled thermoses.
Each floor has a kitchenette so residents can freely prepare tea or coffee. (Participant 11 – Lead Carer)
Everyone then has, for example, next to each bed on their bedside table, their own water next to them. (Participant 20 – Care worker)
They have a kitchenette in their room. (Participant 31 – Active ageing facilitator)
Discussion
A hydration-promotion culture was highly evident across the participating homes, where the routine provision of fluids during various care activities is rooted in their daily practice. Despite a lack of awareness of any existing policies or guidelines specifically relating to hydration care within all care homes, staff were very mindful of the importance of promoting fluid intake and avoiding adverse events in their elderly population. This was also demonstrated in the strong narratives about the pride staff take in keeping residents well-hydrated and avoiding episodes of dehydration that require hospitalisation. The latter was considered a benchmark and an indicator of the quality of care they provide. However, in our study, staff reported a lack of ongoing training in relation to hydration care and the knowledge they held was mainly acquired through pre-registration training. Of note is that there was lack of consistency in relation to daily fluid targets, with staff reporting anything between 0.5 L to 3.0 L daily for residents with no fluid restrictions, despite European guidelines recommending daily fluid targets of 2.5 L for men and 2.0 L for women (European Food Safety Authority 2010). These findings are consistent with those of Cook et al. (2019), highlighting a possible knowledge gap amongst staff which could result in challenges in meeting residents’ daily hydration requirements. Gaps in current literature about how policies and procedures influence day-to-day hydration care in residential elderly settings are also evident (Bunn et al. 2015; Bunn, Hooper, and Welch 2018; Oates and Price 2017). Previous literature substantiates the need for further robust cohort studies investigating the effect of policies and training in improving fluid intake and hydration status in elderly residential settings (Bunn et al. 2015’ Bunn, Hooper, and Welch 2018). Our study supports this premise and adds that, in the local context, there is a further need for staff training and implementation of clear and accessible guidelines, policies, and/ or procedures in relation to hydration care within elderly residential settings.
Strategies for monitoring fluid intake varied across the care homes and included assessment of signs and symptoms of dehydration, monitoring of designated water bottles and stocks of water bottles, blood analysis, seeking feedback from residents, intake and output charting and documentation, with no one home implementing all these strategies collectively. These results reflect the diverse approaches cited in other studies with regard to fluid intake assessment and identification of low fluid consumption or dehydration (Bunn et al. 2015; Hart, Marsden, and Paxman 2020; Jimoh et al. 2019; Wilson et al. 2019). It is not surprising that different homes adopt different strategies to monitor fluid intake. Of note, however, is that recent evidence suggesting that observing for signs and symptoms of dehydration may be ineffective (Bunn and Hooper 2019) since dehydration can only accurately be measured through serum or plasma osmolality (Bunn 2019). Obtaining a venous blood sample is an invasive procedure, therefore it may not be favoured as the best approach to monitor the fluid status of older adults. Considering this recent evidence, we maintain the view that continuous training opportunities and clear policies and guidelines for staff in relation to monitoring fluid status and identifying residents at risk of dehydration is essential in ensuring residents are meeting their fluid requirements. As identified by Oates and Price (2017), there is a lack of standardised assessment tools to monitor fluid intake or changes in hydration status of older people, in view of different patient groups and settings. This study did not seek to investigate the effectiveness of monitoring strategies employed by staff and, since current literature lacks the required methodological rigour to draw any conclusions (Bunn et al. 2015; Hart, Marsden, and Paxman 2020), future research should focus on establishing an evidence-based approach to monitoring hydration status and identifying residents at risk of dehydration in an attempt to minimise the number of hospital admissions locally.
In this study, intake and output charting and documentation were predominantly utilised when residents were noted to have decreased fluid intake, particularly if they were refusing fluids, suffered from dementia, or had a high level of dependency. It seems plausible that the latter challenges instigate staff to be more vigilant in supporting these residents to achieve their hydration requirements. However, similar to findings from the feasibility study (Micallef, Vella, and Sciberras Narmaniya 2021), participants also acknowledged the difficulty in monitoring the fluid intake of independent residents. This cohort of residents were less of a concern to staff in relation to achieving their hydration requirements, since they were able to help themselves to drinks whenever they required. Thirst in older people may not be relied on as an indicator of dehydration (Shaw and Cook 2017) and residents are often concerned about the risk of incontinence resulting in restricting their fluid intake (Wilson et al. 2019). These barriers place independent residents at risk of dehydration, and it is reiterated that emphasis on the importance of not overlooking this group of residents be highlighted. Organisational factors, such as staffing issues and the time-consuming nature of hydration support (Cook et al. 2019; Mentes 2006) often lead to staff having to choose between more urgent care activities (Godfrey 2012). However, there is some research to suggest that residents completing their own drinks diaries is a potential assessment approach that was found to be more accurate than documentation completed by staff (Jimoh, Bunn, and Hooper 2015). The latter could provide a potential solution to the barriers identified here in relation to monitoring independent residents. However, this requires further research, employing robust and rigorous methods to establish the effectiveness and implementation of such approaches in local care homes.
Limitations
Although this study contributes valuable insight into the local situation in relation to hydration practices as regards the residential care of older adults, the inclusion of six care homes and the use of convenience sampling limits transferability of results. This was mitigated by recruiting one home from each region of the Maltese islands. However, the findings may still not be representative of hydration practices and approaches in other residential care home settings. This study did not assess fluid intake or hydration status of residents but reported staff views of hydration practices and approaches. Moreover, residents’ perspectives were not explored. Investigating these areas may provide further insight into the strategies, facilitators, and barriers in achieving optimal hydration requirements for residents.
Conclusion
A hydration-promotion culture was demonstrated through various practices in the care homes. Staff were very mindful of the importance of promoting fluid intake and avoiding adverse events in older adults. However, the variation of daily fluid targets to meet residents’ hydration requirements emphasises the need to explore in more depth whether Maltese care homes have clear hydration policies and how these influence hydration approaches to care and ultimately residents’ hydration status. Different strategies for monitoring fluid status were identified in this study. Despite recent evidence suggesting that assessing for signs and symptoms of dehydration in older adults may be ineffective, this was one of the strategies used by staff in local care homes. This study therefore highlights the need for staff training and the implementation of clear and accessible guidelines, policies, and/or procedures in relation to hydration care within residential care settings for older people. Care homes should consider providing clear information to staff about the assessment of residents’ hydration needs and set standards that can be integrated in routine practice for ensuring the optimal hydration of residents. Difficulty in monitoring the fluid intake of independent residents was highlighted in this study and therefore it is imperative that this group of residents should not be overlooked in view of the risk of dehydration. Further research into innovative approaches of self-monitoring may be a potential solution that requires further research in the local setting. Employing robust and rigorous methods to establish the effectiveness and implementation of such approaches would help in making valid contributions to the local evidence-base on hydration care within this context.
References
Allen, V.J., Methven, L. and Gosney, M. 2013. ‘The influence of nutritional supplement drinks on providing adequate calorie and protein intake in older adults with dementia’, Journal of Nutrition, Health and Aging, 17, 752-755.
Braun, V. and Clarke, V. 2006. ‘Using thematic analysis in psychology’, Qualitative Research in Psychology, 3, 77-101.
Bunn, D., Jimoh, F., Wilsher, S.H. and Hooper, L. 2015. ‘Increasing fluid in- take and reducing dehydration risk in older people living in long-term care: a systematic review’, Journal of American Medical Directors Association, 16(2) 101-113.
Bunn, D., Hooper, L. and Welch, A. 2018. ‘Dehydration and malnutrition in residential care: recommendations for strategies for improving practice derived from a scoping review of existing policies and guidelines’, Geriatrics, 3, 77-90.
Bunn, D. 2019. ‘Effective hydration care for older people living in care homes’, Nursing Times, 115, 54-58.
Bunn, D.K. and Hooper, L. 2019. ‘Signs and symptoms of low-intake dehydration do not work in older care home residents – DRIE Diagnostic Accuracy Study’, Journal of American Medical Directors Association, 20, 963-970.
Cook, G., Hodgson, P., Hope, C., Thompson, J. and Shaw, L. 2019. ‘Hydration practices in residential care homes for older people’, Journal of Clinical Nursing, 28, 1205-1215.
European Food Safety Authority 2010. ‘Scientific opinion on dietary reference values for water’, European Food Safety Authority Journal, 8, 1-48.
Formosa, M. and Farrugia Jones, C. 2017. ‘An overview of patient cases which have problems with discharge from Mater Dei Hospital’, Malta Medical Journal, 1, 22-25.
Formosa, M. 2019. ‘Measuring and Modelling Demographic Trends in Malta: Implications for Ageing Policy’, International Journal Ageing in Developing Countries, 4, 78-90.
Gasper, P.M. 2011. ‘Comparison of four standards for determining adequate water intake of nursing home residents’, Research and Theory for Nursing Practice: An International Journal, 25(1), 11-22.
Godfrey, H., Cloete, J., Dymond, E. and Long, A. 2012. ‘An exploration of the hydration care of older people: a qualitative study’, International Journal of Nursing Studies, 49(10), 1200- 1211.
Hart, K., Marsden, R. and Paxman, J. 2020. ‘Generation of thirst: a critical review of dehydration among older adults living in residential care’, Nursing and Residential Care, 22, 1-12.
Hooper, L., Bunn, D.K., Downing, A., Jimoh, F.O., Groves, J., Free, C., Cowap, V., Potter, J.F., Hunter, P.R. and Shepstone, L. 2016. ‘Which Frail Older People Are Dehydrated? The UK DRIE Study’, Journal of Gerontology, 71, 1341-1347.
Hospital Activity Analysis (HAA) 2021. ‘Email to Hydration Practices Team MCAST’. 23 September.
Jimoh, F.O., Bunn, D. and Hooper, L. 2015. ‘Assessment of a Self-Reported Drinks Diary for the Estimation of Drinks Intake by Care Home Residents: Fluid Intake Study in the Elderly (FISE)’, The Journal of Nutrition, Health and Aging, 19(5) 491-496.
Jimoh, O.F., Brown, T.J., Bunn, D. and Hooper, L. 2019. ‘Beverage intake and drinking patterns – clues to support older people living in long-term care to drink well: DRIE and FISE studies’, Nutrients, 11(2), 447-461.
Kingston, T. 2017. ‘Promoting fluid intake for patients with dementia or visual impairments’, British Journal of Nursing, 26, 98-99.
Lesnik, A. and Bevac, S. 2015. ‘Identification of dehydration in the elderly treated in emergency unit: action research’, Slovenian Nursing Review, 49, 144-148.
Mentes, J.C. 2006. ‘A typology of oral hydration problems exhibited frail nursing home residents’, Journal of Gerontological Nursing, 32(1), 13-19.
Micallef, F., Vella, M., Sciberras Narmaniya, A., Cook, G. and Thompson, J. 2021. ‘An exploration of hydration practices in Maltese residential care homes for older people’, Nursing and Residential Care, DOI:10.12968/nrec.2021.23.11.3 .
Murray, S. 2017. ‘Identifying and managing dehydration in care homes’, Nursing and Residential Care, 19, 197-200.
Oates, L.L. and Price, C.I. 2017. ‘Clinical assessments and care interventions to promote oral hydration amongst older patients: a narrative systematic review’, BMC Nursing, 16(4), DOI:10.1186/s12912-016-1095-x.
Organisation for Economic Cooperation and Development 2020. ‘State of Health in the EU Malta – Country Health Profile 2021’. Available at: https://www.oecd-ilibrary.org/social-issues-migration-health/malta-country-health-profile-2021_cd4b1ed7-en (accessed 26 October 2022).
Paulis, S., Everink, I., Halfens, R., Lohrmann, C. and Schols, J. 2018. ‘Prevalence and Risk Factors of Dehydration Among Nursing Home Residents: A Systematic Review’, Journal of American Medical Directors Association, 19, 646-657.
Robinson, S.B. and Rosher, R.B. 2002. ‘Can a Beverage Cart Help Improve Hydration?’, Geriatric Nursing, 23, 208-211.
Shaw. L. and Cook, G. 2017. ‘Hydration practices for quality dementia care’, Nursing and Residential Care, 19, 620-624.
Simmons, S., Alessi, C. and Schnelle, J. 2001. ‘An intervention to increase fluid intake in nursing home residents: prompting and preference compliance’, Journal of American Geriatrics Society, 49, 926-933.
Vandervoort, A., Van den Block, L., Van der Steen, J.T., Volicer, L., Vander Stichele, R.H., Houttekier, D. and Deliens, L. 2013. ‘Nursing Home Residents Dying with Dementia In Flanders, Belgium: A Nationwide Post-Mortem Study on Clinical Characteristics and Quality of Dying’, Journal of American Medical Directors Association, 14, 485-492.
Vella, M., Sciberras Narmaniya, A. and Micallef, F. 2021. ‘Hydration practices in older adult residential care homes: a scoping review’, MCAST Journal of Applied Research and Practice, 5(2), 58-85.
Wilson. J., Bak, A., Tingle, A., Greene, C., Tsiami, A., Canning, D., Myron, R. and Loveday, H. 2019. ‘Improving hydration of care home residents by increasing choice and opportunity to drink: a quality improvement study’, Clinical Nutrition, 38(4), 1820-1827.
Wolff, A., Stuckler, D. and McKee, M. 2015. ‘Are patients admitted to hospitals from care from care homes dehydrated? A retrospective analysis of hypernatraemia and in-hospital mortality’, Journal of the Royal Society of Medicine, 108, 259-265.
Woodward, M. 2007. ‘Guidelines to Effective Hydration in Aged Care Facilities. Heidelberg Repatriation Hospital (Heidelberg Heights, Victoria)’. Available at: www.mcgill.ca/ familymed/files/familymed/effective_hydration_in_elderly.pdf (accessed 27 October 2022).
Wotton, K.G., Crannitch, K. and Munt, R. 2008. ‘Prevalence, risk factors and strategies to prevent dehydration in older adults’, Contemporary Nurse, 31, 44-56.